New to Insulin English- Why do I need Insulin?
It is a hormone produced by pancreas to regulate the levels of glucose in the blood. In absence of insulin our body cells cannot use glucose as a source of energy. When you have diabetes, your body doesn’t make insulin or the insulin you do make doesn’t work right. Hence, you need external insulin. You can get the insulin you need by injecting it with an insulin pen, a syringe, or insulin pump. Taking insulin will: Help you to control your sugar levels Give you energy Help you to stay healthy

New to Insulin English- Insulin Secretions in Body
Insulin is secreted during fasting state known as Basal Insulin. The secretion of insulin increases in response to increased blood glucose levels after taking food. This process is affected in diabetes for which insulin from outside needs to be injected.
New to Insulin English- What is Hypoglycemia?
Hypoglycemia is a condition characterised by abnormally low blood glucose levels, usually less than 70 mg/dl. This can happen if you: Do over exercise Don’t eat enough Skip a meal Take too many medicines However, it is important to talk to your health care provider about your individual blood glucose targets, and what level is too low for you.

New to Insulin English- What should I do when Hypoglycemia occur?
When You Have Low Blood Sugar First, eat or drink 15 grams of a fast-acting carbohydrate, such as: Three to four glucose tablets One tube of glucose gel Four to six pieces of hard candy (not sugar-free) 1/2 cup fruit juice 1 cup skim milk 1/2 cup soft drink (not sugar-free)
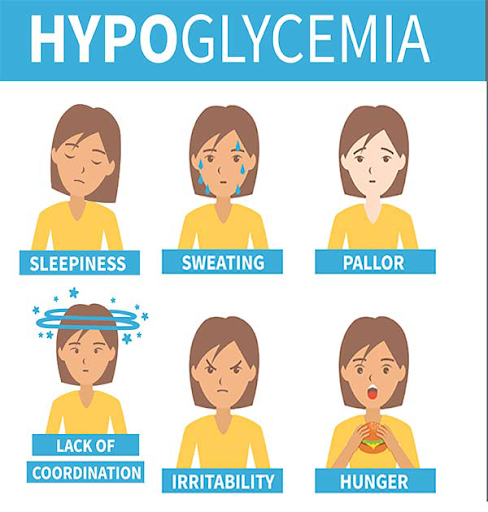
New to Insulin English- What are the signs or symptoms of Hypoglycemia?
Shaking Sweating Dizziness Hunger Fast heartbeat Blurry vision Headache Weakness or fatigue If you have a low blood sugar problem, it’s important to eat or drink 15 grams of fast acting sugary food right away, such as; ½ can of regular (not diet!) soda 1 tablespoon (or two packets of a real sugar) 3 hard candies that you can eat quickly
New to Insulin English- Nocturnal Hypoglycemia – Night Time Hypo
Nocturnal hypoglycemia or night time hypos are common in people who treat their diabetes with insulin. Symptoms are usually only realised once waking up from a hypo. Due to their nature, you will usually only find out about having a hypo during the night after waking up from a hypo. Therefore people may not even be aware that they are having night time hypos, so it’s useful to be able to spot the signs and symptoms of when nocturnal hypoglycemia may be taking place. Whilst nocturnal hypoglycemia is most common in insulin users, it can also occur for people who take oral anti-diabetic drugs.

New to Insulin English- Symptoms of night time hypoglycemia
Sometimes you may wake during an episode of nocturnal hypoglycemia. However, if you don’t, you may notice one or more of the following indications that hypoglycemia may have occurred whilst you were asleep. Restless sleep Vivid dreams or nightmare Morning headache Night sweats Mood changes Fatigue Convulsions

New to Insulin English- Nocturnal hypoglycemia in children
For parents of children with diabetes, nocturnal hypoglycemia can be particularly worrying. Parents of diabetic children may wish to check their child’s neck whilst they are sleeping if they are worried that night time hypoglycemia may be occurring.

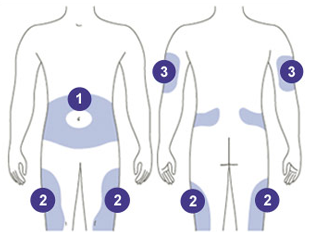
New to Insulin English- How should I take Insulin?
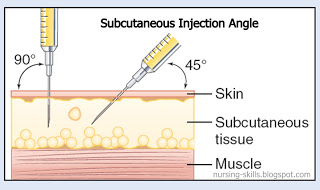
Insulin works best when you inject it into the fatty parts of the body just under the skin. Before you leave the clinic, ensure that you know how to: Prepare insulin Inject insulin Rotate injection site

New to Insulin English- Which are the insulin delivery devices?
There are different devises to deliver insulin into your body through; syringes, insulin pen, insulin pump, and i-Port are different options for insulin delivery. Syringe- Insulin syringes are different from normal one. They are thinner, have almost pain less needle and come with removable needle guard. The outer side of the syringe is marked with lines to assist you to withdraw correct amount of insulin. Pen- It is composed of an insulin cartridge (integrated or bought separately) and a dial to measure the dose, and is used with disposable pen needles to deliver the dose. Insulin pens offer several significant advantages over insulin syringes: Ease of handling Accuracy
New to Insulin English- How to inject using a syringe?
Wash hands with warm & soapy water If using cloudy insulin, roll the bottle (do not shake) between hands. Clean rubber stopper of insulin bottle with alcohol. Fill syringe with air equal to the number of units of insulin you will be taking. Insert needle into the bottle and push air into the insulin bottle. Turn syringe and bottle upside down and draw out your dose of insulin. Insert the needle into the skin Press the plunger on the end of the syringe to deliver the dose
New to Insulin English- How to inject using a pen?
Screw or click on a new pen needle. If necessary, prime the pen to remove any air from the needle Turn the knob on the end of the pen (or "dial") to the number of units needed Insert the needle into the skin Press the button on the end of the pen to deliver the dose Count to five or ten depending on dose injected Remove used pen needle for disposal Some tips for using the syringe and Pen for insulin delivery: Shorter needles mean lesser injection discomfort. However, injection depth affects how quickly insulin takes effect. Coordinate syringe size (e.g., 1cc, 1/2cc, 3/10cc) to match insulin dose. Do not re-use a syringe/pen needle. Do not share a syringe. Dispose of used syringes/ pen needle properly